Simvastatin Does Not Enhance Escitalopram
Data Show Simvastatin Does Not Enhance Escitalopram Response in Comorbid Depression and Obesity
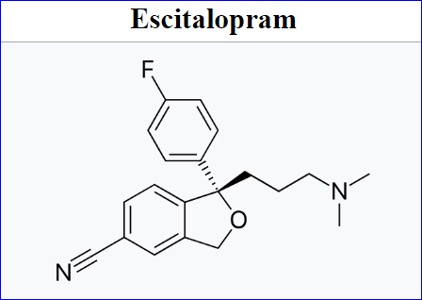
Simvastatin did not enhance antidepressant effects when added to escitalopram in patients with MDD and obesity, despite improving cardiovascular risk factors. Previous studies suggested potential antidepressant benefits of statins, but randomized trials have shown inconsistent results, particularly in patients with MDD and obesity.
Statins such as simvastatin do not have additional antidepressive effects in combination with standard escitalopram treatment in patients with comorbid major depressive disorder (MDD) and obesity.
Results from an extensive study (NCT04301271) published in JAMA Psychiatry demonstrate that adding simvastatin (Zocor; Merck & Co.) to escitalopram (Lexapro; Forest Laboratories) did not elicit additional antidepressive effects in patients with comorbid major depressive disorder (MDD) and obesity despite improving cardiovascular risk, affirming that statins should not be relied on to help manage depression.
Possible Associations Between Statins and Antidepressive Effects
Previous small, experimental studies have described potential benefits of statins in MDD. One study group determined through an online observational study in 2021 that statins could influence an individual’s emotional biases, which are a marker for depression risk. Recent meta-analyses of cohort studies investigating the association have yielded differing results but suggested possible benefits of statins in lowering depression risk.
Randomized clinical trials are necessary to truly elucidate the effectiveness of statins in combination with standard antidepressants. Though some small, randomized trials have reported benefits, others have failed to demonstrate any positive effects. Furthermore, no randomized trial has investigated these effects in patients with MDD and comorbid obesity, a difficult-to-treat population that often exhibits chronic MDD and is more difficult to treat with standard methods. Determining the association using a large, randomized population could have major implications for the treatment of both MDD and obesity.
“If statins really did have this antidepressive effect, we could kill 2 birds with 1 stone,” Professor Christian Otte, MD, the trial’s lead author, said in a news release accompanying the results. “Depression and adiposity, or obesity, are among the most common medical conditions globally. And they actually often appear together: those who are obese are at a higher risk of depression. In turn, those with depression are at a higher risk of obesity.”
Despite Improving Metabolic Factors, Statins Have No Impact on Depression
For this 2-arm, double-blind, placebo-controlled, multicenter trial, the study authors randomized 160 patients (placebo: n = 79; simvastatin: n = 81) to receive either simvastatin 40 mg per day or placebo as an add-on to escitalopram. Patients received escitalopram at 10 mg for the first 2 weeks, with doses then increased to 20 mg until the study concluded. The primary outcome measured by the authors was change in Montgomery-Åsberg Depression Rating Scale (MADRS) score from baseline to week 12.
In both patient groups, MADRS scores from baseline to week 12 decreased substantially (simvastatin: –13.97 points [95% CI, –15.88 to –12.06]; placebo: –13.50 points [95% CI, –15.41 to –11.58]). Patients in the intent-to-treat sample demonstrated no major treatment effects of add-on simvastatin compared with add-on placebo in MADRS scores (MMRM least squares mean difference: 0.47 points [95% CI, –2.08 to 3.02]; P = .71), with preplanned sensitivity analyses confirming the result, according to the investigators.
Key secondary end points were also investigated. Patient-reported depression severity, as measured by the Beck Depression Inventory II (BDI-II) score, was reduced in both treatment cohorts, but there was no significant treatment effect for simvastatin. Notably, there were no meaningful group differences in any of the exploratory end points for quality of life, social functioning, or global impression of change from the participants’ or clinicians’ point of view, reaffirming the lack of simvastatin effects on mental health outcomes.
Despite the lack of effect on mental health end points, treatment with simvastatin had robust positive effects on metabolic health. Simvastatin helped reduce low-density lipoprotein and total cholesterol levels compared with placebo, suggesting strong adherence to the regimen among participants and the beneficial role statins can still play in this comorbid population.